Posted on June 19, 2024 by Sally-Anne Turner
As obesity levels are rising across the world, clinicians and medical professionals are emphasizing the fact that our weight can have a significant effect on our wellbeing, both physically and mentally.
That’s why it’s absolutely vital that we boost public health knowledge regarding obesity and weight health, so that we know when our weight is becoming a problem, and how we can fix it.
That’s where handy tools like the BMI comes in, so we can identify whether or not our weight is healthy or unhealthy, and whether we need to address this to improve our overall weight health. Here at Bodyline, we’d like to expand on what the BMI is, how it is used to identify obesity, and how we can help to lower the BMI if it is getting too high.
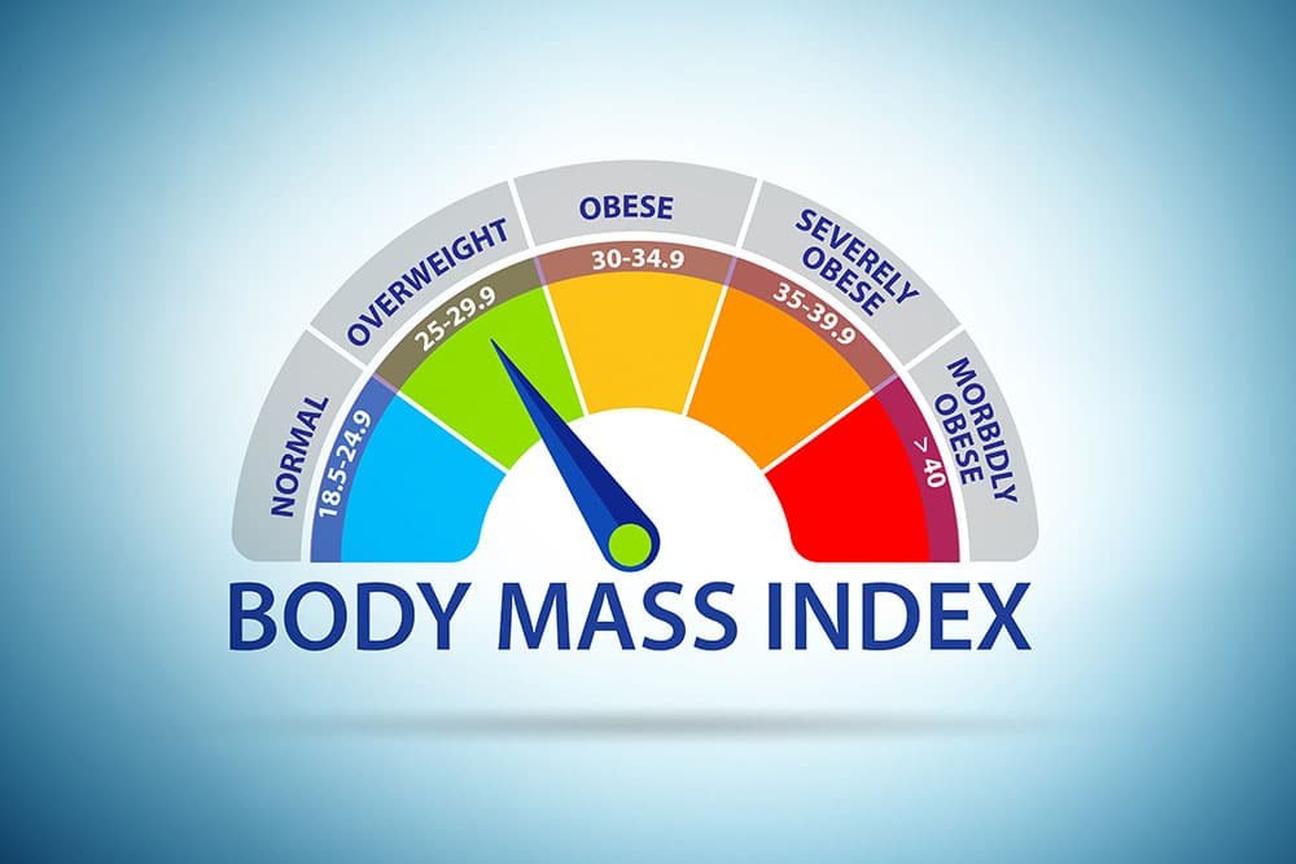
Body Mass Index (BMI) is a numerical value that can provide an estimate of an individual's overall weight health. It is calculated by dividing a person's weight in kilograms by the square of their height in meters. The resulting number is then categorized into different BMI ranges to assess if a person is underweight, normal weight, overweight, or obese.
The BMI was invented in the 1800’s by a male scientist, who based his theory on a group of men’s weights and heights, so some researchers believe the BMI is not always the best way to identify weight health.
However, when paired with other identifiers such as waist circumference and blood pressure, it can be a good tool to start with if you are concerned about your weight and want to work out your health levels.
BMI is widely used as a screening tool to assess weight health on a population level. While it does not directly measure body fat percentage or account for individual variations in muscle mass, it serves as a useful indicator for the general population.
BMI is often associated with health risks, as certain BMI ranges have been linked to an increased likelihood of developing weight-related health conditions, such as heart disease, diabetes, and certain types of cancer.
Calculating your BMI is a straightforward process. Here's a step-by-step guide:
Or, you can use the handy online NHS calculator for BMI here.
A BMI of 30 or higher is generally considered obese. However, it's important to note that BMI is not the sole determinant of obesity or overall health. Other factors, such as body composition, waist circumference, and distribution of fat, can also influence an individual's health risks.
Obesity, however, is not just a result of lifestyle choices, it can be caused by genetics, age, hormones, medical history, and ethnicity.
Katie Illingsworth is Bodyline’s resident nutritional therapist alongside her role as nurse prescriber. Having experienced weight health related problems herself, she is passionate about helping those struggling with weight loss.
“I was struggling with my own weight issues, but through my own learning and understanding, I stopped being so hard on myself because hormonally something was out of whack. The research suggests that when your BMI is over 40, you're so hormonally dysregulated, you will not lose weight by yourself. That’s why medical and clinical support can be so important in treating weight health.
“Everyone at Bodyline has probably experienced their own weight health issues or hormonal issues, and because it's a predominantly female led company, we can really relate when it comes to the hormone health advice. We acutely understand it.”
Lowering your BMI from the obesity range requires a comprehensive approach that focuses on sustainable lifestyle changes. Luckily, there are now brand-new medical interventions for the treatment of obesity in the form of GLP-1 injectable therapies, as well as established successful oral treatments that have helped millions transform their bodies and change their lives for the better.
The Medicines and Healthcare products Regulatory Agency (MHRA) recently approved both semaglutide (WeGovy) and tirzepatide (Mounjaro) to be prescribed as a treatment for obesity. Those eligible are people with a BMI of 30 or above, or of 27 and over and living with weight health problems like heart disease or diabetes.
These game-changing treatments have seen users lose on average more than 15% of their starting body weight through clinical trials and are a very promising choice to tackling obesity. In fact, one large study of 22 trials comparing tirzepatide and semaglutide found that tirzepatide was superior to semaglutide in terms of controlling blood sugar levels and promoting weight loss.
However, they are not magic solutions, they must be used alongside healthy lifestyle changes and within fully supported and supervised medical programmes to achieve the most sustainable and positive results.
Here are some strategies that should be adopted alongside medical treatments to lower BMI and improve overall weight health:
Remember, weight loss should be approached in a healthy and balanced manner. It is important to set realistic goals, celebrate progress, and prioritise overall well-being rather than focusing solely on the number on the scale.
At Bodyline Clinic, we offer medically supervised weight loss programmes tailored to your unique needs. Our experienced healthcare professionals provide comprehensive guidance, support, and monitoring to help you achieve your weight loss goals. Contact us today or call 0800 995 6036 to start your journey to a healthier, happier you.